Focus on mycotoxins
DLG Expert report 2-2016
Mycotoxins (toxic substances produced by fungi) are a significant hygiene problem in both foods and feeds worldwide. These are secondary metabolic products formed by mould fungi that have a toxic effect in various ways already in very low doses in vertibrates and humans. In humans they hardly cause acute damage to health, but they can be carcinogenic or mutagenic. Illnesses caused by mycotoxins are generally termed mycotoxicosis. These must be distinguished from mushroom poisoning caused by toxins formed by various higher fungi, for instance the amatoxins and phallotoxins contained in the amanita. This kind of toxin is not counted among the mycotoxins in the narrower sense.
The kingdom of fungi
In the system of living organisms, fungi form a separate category in the domain of the eukaryotes, those organisms whose cells contain a nucleus. The world of fungi includes both single-cell organisms, such as for instance bakers’ yeast (Saccharomyces cerevisiae) and multi-cellular organisms such as mould fungi and pillar fungi. Mould fungi – or short moulds – are a systematically inhomogeneous group of filamentous (thread-shaped) fungi. While most mould fungi are fairly inconspicuous, some of them are of particular significance for humans, for instance as human parasites or producers of poisons (mycotoxins) in spoiled foods. However, special moulds are also used to produce foods (e.g. Camembert, Roquefort, mould salami) and to produce food additives (e.g. citric acid) and pharmaceuticals (e.g. antibiotics). Since the 1980s quorn – a low-fat food rich in fibers and protein – has also been on the market. It is gained from targeted fermentation and subsequent processing of the mould fungus Fusarium graminearum and is used as a meat substitute product.
Mycotoxins
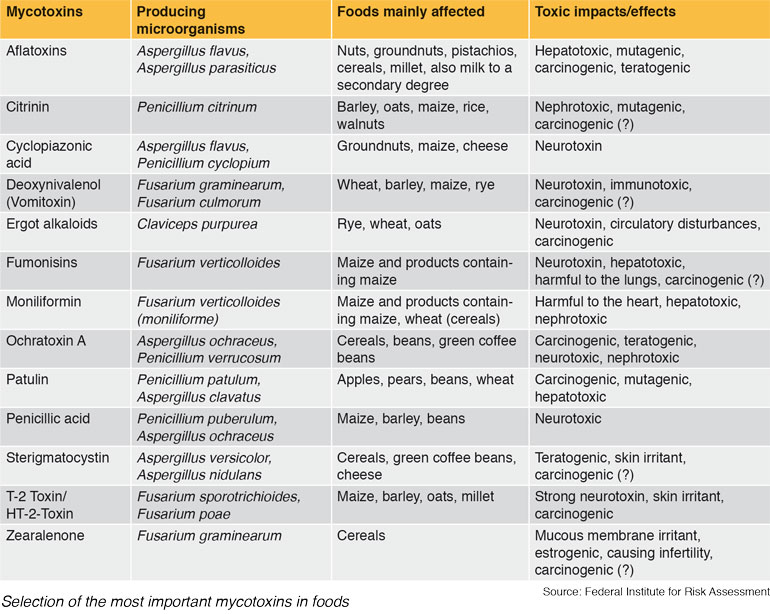
Mycotoxins is a collective term for a group of natural, low-molecular, metabolic products of mainly of lower order mould fungi (Micromycetes), that are toxic for humans and animals and partly also for plants and even for other microorganisms. The term derives from the Greek “myko” (fungus) and the Latin “toxicum” (poison). Today over 400 toxic fungal metabolites are counted among the group of mycotoxins, but it is estimated that there are several thousand mycotoxins. According to the current status of knowledge, however, only around 20 of them occur frequently and in critical concentrations in foods. The table shows the most important of these mycotoxins relevant for food safety, their main producers, the main fields of occurrence and their toxic effects.
It is not yet clear what function the secondary metabolic products in general and the mycotoxin formation specifically play in the metabolism of mould fungi. It is assumed that metabolic control functions, evolutionary reserve functions and ecological aspects act in interplay with other microorganisms, such as for instance other fungi, bacteria or other monocellular organisms, in order to eliminate these for example as competitors.
As the mycotoxins are formed in the secondary metabolism of the moulds, by contrast with the substances in primary metabolism they are not encountered in all types of moulds. Instead, the production of a certain toxin may be restricted to a few particular species, but it can also be encountered in many species of several genera. In practice, this means that when mould occurs spontaneously on a food, it must always be expected that there is a risk of mycotoxin formation, but this need not necessarily be the case. Consequently a food that already displays distinct growth of moulds must not necessarily also contain mycotoxins. Fundamentally the mycotoxins are formed during or following the growth of mould fungi. Here too, strong fungal growth need not necessarily be connected with intensive toxin formation. Conversely, however, low fungal growth can certainly be linked with strong toxin formation. This is because the formation of mycotoxins is subject to pronounced regional and seasonal fluctuation ranges. Thus they are often only formed under certain temperature/moisture and pH conditions, in the case of rich nutrient supplies, or in certain development phases of the mould fungus, and interactions with other fungi are also observed. To form toxins, substrates that are rich in carbohydrates of complex composition are generally preferred, such as is often the case in plant substrates. When mycotoxins are formed, it often happens that not just one defined substance is found, but instead a whole family of chemically-related substances.
Mycotoxins – not a new problem
As mould fungi species that form mycotoxins are found worldwide, foods infected with mould and hence mycotoxins have accompanied humans since the beginning of time. A mycotoxicosis, namely ergotism, also known as Saint Anthony’s Fire, is already described in the Bible (3rd Book of Moses 14:34-48). This illness caused by consumption of ergot then claimed hundreds of thousands of human lives from the Middle Ages right into modern times.
However, fusariotoxins were reportedly also a significant cause of illness at this time. At the end of the 19th century fatal cases of poisoning occurred among people in Russia that were brought into causal contact with the consumption of cereals which were only harvested after the winter and were contaminated to a high degree with fusaria and probably also their toxins. During World War II, thousands of people in the Soviet Union fell victim to a disease known as Alimentary Toxic Aleukia (ATA), which was also attributable to the consumption of cereals that had been infected with fusaria over the winter. The T2 toxin from the group of trichothecenes formed by fusaria, which was found in a concentration of up to 2.5% in the Russian cereal samples, could only be identified years later as the real cause of the disease. The fact that science originally had difficulties in connection with the mycotoxins was above all due to the circumstance that methods first had to be developed for obtaining sufficiently precise information about the concentration ranges in which mycotoxins are normally present in the affected foods.
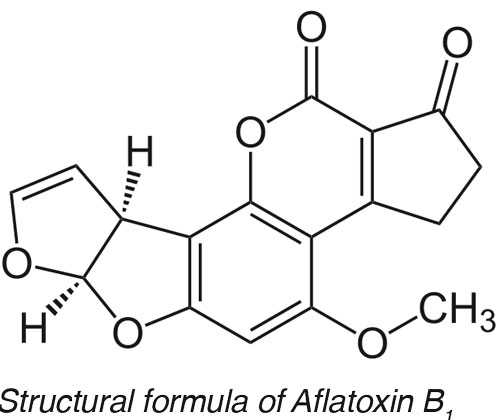
However, mycotoxins only moved into the focus of public and scientific interest in the 1960s when in England around 100,000 young turkeys died due to mouldy groundnut meal (Turkey X Disease). The search for the cause led to the discovery of the aflatoxins, which were named after their first known producer, namely Aspergillus flavus.
Toxicity
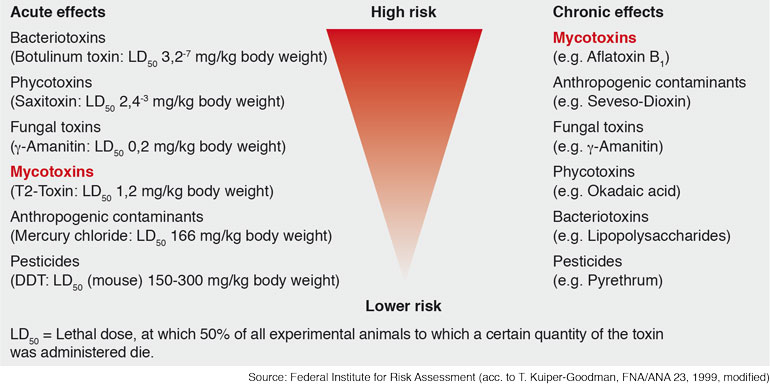
While most bacteriotoxins can trigger antibody reactions due to their protein nature, this is not the case with mycotoxins. As a result of their low molecular weight, they do not lead to the creation of antibodies.
Mycotoxins can have an acute and/or chronic toxic effect depending on their nature. By acute toxicity we understand the harmful effects of a substance that occur within a certain time – immediately or normally within 14 days – after administration of a single dose. Chronic toxicity on the other hand covers the toxicity of a substance that is repeatedly absorbed over a relatively long period. By comparison with other toxins, the acutely toxic effects of mycotoxins on humans can generally be neglected.
Acute intoxications occur above all in animals, especially in farm animals such as pigs and cows. Symptoms caused by this may be vomiting, changes in the blood count, harm to organs such as liver and kidney (hepatotoxic or nephrotoxic), attacks on the central nervous system (neurotoxic), skin and mucous membrane damage in the case of contact, impairment of the immune system (immunosuppressive) and hormone-like effects. Neurotoxins can lead to trembling and to cramps, and ultimately to death.
Chronic symptoms generally occur after more than six months, whereby both substance-cumulative and effect- cumulative symptoms can be observed. Provided that they do not concern genotoxic effects such as mutagenity or cancerogenity, chronic effects are dependent on a threshold, i.e. a NOEL (No observed Effect Level) can be stated, below which no toxic effects can be observed. According to the present status of scientific knowledge this is not possible for substances with genotoxic effects, as a genotoxic effect can theoretically be triggered already by a single molecule. Above all cancerogenic (cancer-triggering), mutagenic (causing genetic damage) and teratogenic (causing malformations of embryos) effects are described as late consequences due to chronic intake of mycotoxins.
Some of the mycotoxins occurring in foods can accumulate in specific target organs (above all in the liver and kidneys) in our body and from case to case can also be transformed into more dangerous substances. The latter applies e.g. to the aflatoxins.
Contamination of foods
Although it is possible to absorb mycotoxins already via respiratory air when working with organic materials such as foods, feeds or wastes, humans are chiefly threatened via contaminated foods. Normally three different cases are distinguished with regard to contamination: - We speak of primary contamination when the plant raw material was infected by toxin-forming mould fungi already in the field (e.g. ergot in cereals). In the course of processing infected raw materials, the fungus mycelium can be reduced and finely distributed in such a way that it is no longer visible in the end product and contamination is no longer visually recognisable. - Secondary contamination occurs when moulds are growing during storage, transport or further processing of food. A fundamental risk of mycotoxin formation can be recognised by consumers too as a result of the growing fungal colony which is often also characteristically coloured by spore formation.
- Carry over is a term used to describe the situation when productive livestock ingest mouldy feeds containing toxins which are deposited in various organs in unchanged or metabolised form or excreted. This leads to a situation in which food of animal origin – meat, eggs, milk – can also contain mycotoxins without the relevant product being mouldy itself.
According to estimations by the Food and Agriculture Organization of the United Nations (FAO), around 25% of all foods on the earth contain mycotoxins.
If an agricultural raw material or food is contaminated with mould fungi, it should be noted that these grow not only on the surface, but also penetrate deeply into the harvested material or the food with their hyphae, the fungal threads. The fungal toxins are then excreted into the substrate on which they grow, or stored in cells from which they are released when the mycelium – that is the mass of the thread-like hyphae – breaks open. Thus toxins can occur both on and in the foods, which is important with regard to possible decontamination options. The spores of mould fungi can also contain mycotoxins, which explains possible intake via the respiratory air.
Determination of mycotoxins
Both trace analytical methods and quick methods are available for determining mycotoxins. High performance liquid chromatography (HPLC) is generally used to separate the extracts obtained from the food to be examined. Detection and quantification of the mycotoxins are then carried out with the aid of various detectors, such as ultraviolent detectors (UVD) or fluorescence detectors (FLD), or with the aid of mass spectroscopy (MSD). HPLC/ MS/MS is considered to be the most modern method for determining different toxins alongside one another in a single analysis. Switching several mass spectrometer units in series provides a coupling opportunity, the tandem MS, which is also called MS/MS. This is coupled with a chromatographic separation system, the high pressure liquid chromatography. The coupling allows exact identification and quantification of both pure substances and substance mixtures. One great advantage of MS/MS is its speed – measurements can be carried out in milliseconds using this method.
Although the analysis methods discussed so far are very precise, they are extremely time-consuming, which is why fast methods are becoming increasingly more widespread. By fast methods we understand tests that can be carried out quickly and easily and that can supply both qualitative and quantitative results. The examinations can be carried out in the field or in the laboratory and generally do not require expensive equipment. It is therefore no longer possible to imagine routine daily work without them. Typical fast methods are immunological tests such as ELISA and Lateral-Flow tests, as well as chemical examinations such as fluorimetrical methods to determine aflatoxins.
Options for action
Most mycotoxins are chemically very stable and resistant to heat, storage conditions and processing methods. Although a large number of approaches to subsequent detoxification of foods affected by mycotoxins are mentioned in literature, most of these methods are currently not practicable as they are either too time-consuming, too expensive, or have not yet been sufficiently tested. That is why enormous importance is attached to prophylaxis, in other words to preventing such mould formation on foods and feeds.
Approaches in the agricultural sector include the selection of crop rotation, cultivation of site-appropriate varieties, gentle harvesting methods, expedient fertilising, the use of pesticides, avoidance of waterlogging and maintenance of appropriate plant spacing.
The contamination of groundnuts with aflatoxins, partly also with cyclopiazonic acid is a serious problem in practically all cultivation regions in the world, due not least to the respective environmental conditions. Recently, therefore, biological approaches have also been developed to master the problem. One approach here is to apply non-toxigenic strains of Aspergillus flavus on the fields which are supposed to dominantly suppress the toxin-forming strains in their growth. Initial trials under commercial conditions have shown that the aflatoxin content of the groundnuts stored by farmers was reduced by on average 85% and in the shelled, edible groundnuts by up to 98%.
As regards the field of post-harvest treatment and storage of foods and feeds, it is primarily important to control moisture contents and temperature properly. Significant results can also be obtained by mechanical sorting out of irregular products, such as has been demonstrated for instance for cereals, groundnuts, walnuts, almonds and paprika. Further progress can be expected here through the use of sensitive and powerful electronic image identification systems, with the aid of which irregular products can be identified and removed automatically and very quickly.
Maximum level regulations for mycotoxins
According to Art. 2 Section 1 of the Regulation (EEC) No. 315/93, no foods containing a contaminant in an amount which is unacceptable from the public health viewpoint and in particular at a toxicological level may be placed on the market in the EU. As a supplement to this, Art. 2 Section 2 contains a minimising direction according to which contaminant levels are to be kept as low as can reasonably be achieved by following good practices at all the stages. Accordingly work here must proceed in accordance with the ALARA principle (“as low as reasonably achievable”) or the ALATA principle (“as low as technologically achievable”). Should it be necessary for the purpose of consumer protection, according to Art. 2 Section 3 the EU Commission can also determine maximum quantities for certain contaminants.
On this basis maximum levels for mycotoxins applicable throughout the Community were determined in Section 2 of the Annex to Regulation (EC) No. 1881/2006 (consolidated version 2011). This was done for instance for the aflatoxins (Aflatoxin B1 and sum limit levels for the aflatoxins B1, B2, G1 and G2), for ochratoxin A, patulin, and for the fusariotoxins desoxynivalenol, zearalenone and the fumonisins (sum limit levels for the fumonisins B1 and B2). Although according to the recital 38 maximum levels were to be specified for the T-2 and HAT-2 toxins by 01.07.2008, this has still not been done to date. As a matter of principle the maximum values apply for the edible part of the foods listed in the Annex, but there are also exceptions which are explained in the footnotes.
The ban on mixing set out in Article 3 Section 2 of the Regulation (EC) No. 1881/2006 according to which foods which keep to the maximum levels listed in the annex may not be mixed with those that exceed these maximum levels is of practical importance.
Alongside the maximum levels formulated in Regulation (EC) No. 1881/2006, there are additional maximum levels for certain mycotoxins in Germany that are specified in the Contaminant Regulation. This regulation is a historical remainder of the national regulations in which detailed maximum levels were fixed especially regarding mycotoxins. The maximum levels for various contaminants contained in these are gradually being replaced by European regulations. However, as Germany has regulated a large number of maximum levels that do not yet exist at European level, the national provisions will continue to be applied until there are corresponding EU regulations.